
Breast Reconstruction
*DISCLAIMER: THIS SITE CONTAINS GRAPHIC & SURGICAL IMAGES THAT MAY BE DISTURBING TO SOME VIEWERS.
THIS SITE IS INTENDED FOR INDIVIDUALS OVER THE AGE OF 18.
**None of the images on this site have been enhanced or photoshopped.
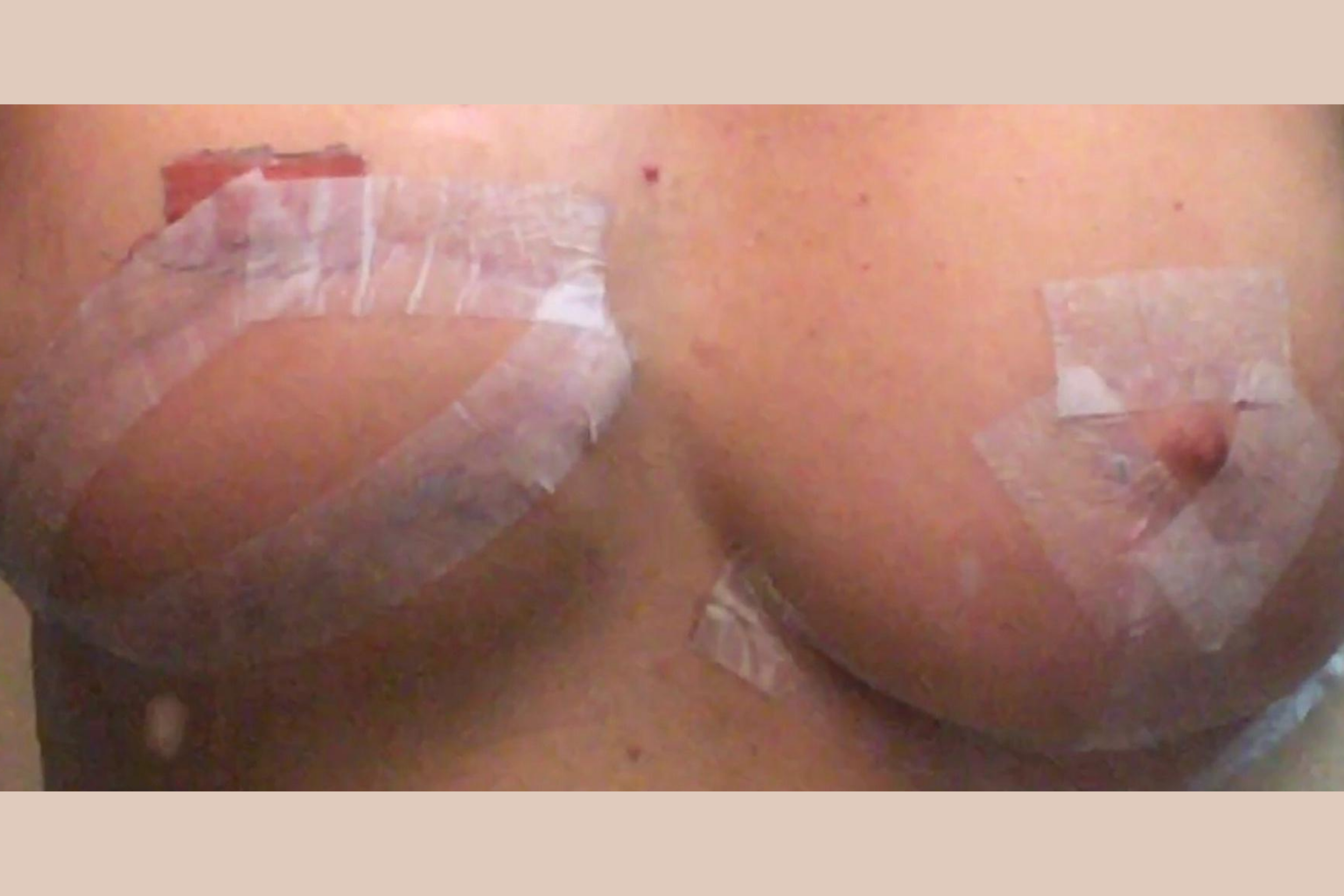
Patient B - 6 weeks Post-Operative Right Latis and Breast Implant, Balancing Left Breast with Breast Lift and Reduction

Before & After Photos
*Tap a patient image to enlarge & view the full series of pre and post-operative images.
Before the Surgery:
+ What are the chances of a woman in Alberta getting breast cancer?
The statistics vary, but in general terms, the life time risk of developing breast cancer, in an otherwise healthy women with no strong family history of breast cancer, is 1 chance in 9-13. If there is a very strong history of female breast cancer in a family, where the mother, and her sisters, and her mother and her sisters all developed breast cancer, you may have what is called the BRACA gene. This is a genetic predisposition to developing breast cancer.
There are 2 types:
- Braca I: predisposes to breast cancer only.
- Braca II: predisposes to breast and ovarian cancer.
There is a blood test that can be done for women with a very strong family history of breast cancer to determine if you are Braca. A consultation with a General Surgeon, on referral from your Family Doctor, is recommended if you suspect you are at risk.
It is very important to do your own breast surveillance. Consider a self-examination of your breasts, once a month in the shower with soap and water, one week after your menstrual cycle, along with an Ultra sound and Mammography at age 40 if there is a positive family history, and at age 50 if no family history is present. These should be repeated periodically, depending on the findings, and your breast density.
A more precise test is an MRI. There may be an indication for this. The General Surgeon you consult with will discuss this further with you.
+ What if I find a breast lump?
You should seek medical advice immediately.
If a breast lump is dangerous and ignored, it could be life threatening.
If you find a breast mass on self-examination, consult your family doctor who will send you for the appropriate investigation along with a consultation with a General Surgeon. If there is a suspicious area on routine ultra sound or mammography, or there is a palpable mass, further investigation with a needle biopsy, or full biopsy, would be arranged and done by the General surgeon. The pathology results of the biopsy will determine what happens next. If the mass or area is benign, ongoing close surveillance will be recommended. If the mass is suspicious or malignant, further treatment will be recommended.
The Operation:
+ What happens if the breast lump biopsy comes back as a breast cancer?
This will depend on the pathological type and size of the breast cancer. It also depends on the results of the investigation tests and the clinical findings.
If it is an isolated breast mass that requires removal, the general surgeon will discuss the surgical options and advise you:
A breast lumpectomy/Segmental resection and radiation to the involved area of the breast. The lymph nodes in the axilla (arm pit) are sampled either before or at the same time (this is called a sentinel node biopsy) as the surgical procedure. This technique preserves a large portion of the natural breast but when healed, the surgery will leave a scar and a contour abnormality and the radiation done after the surgery will create further deforming changes to the breast and axilla.
A traditional mastectomy will leave a flat chest wall with a mastectomy scar. If the lymph nodes are cancer free (the sentinel node biopsy is negative), no further surgery is done. If the sentinel node biopsy is positive and the lymph nodes are involved with cancer, an axillary lymph node dissection will be done to remove most or all of the lymph nodes in the axilla at the same time the mastectomy is done. Radiation is often done after the surgical site is healed. Breast reconstruction after radiation must be delayed for one year from the time the radiation is completed.
A skin sparing mastectomy is a mastectomy which removes the breast tissue, but preserves a large amount of the skin covering the breast. This allows the opportunity for an immediate breast reconstruction done at the same time as the skin sparing mastectomy. This is done when the lymph node sentinel biopsy is negative and no radiation is required. Most often the nipple and a small amount of skin is removed along with the breast, although, there are some circumstances that the nipple may be preserved. This is a discussion the General Surgeon will have before surgery.
** Please refer to Image of Patient A above.
+ What is the difference between an immediate reconstruction and a delayed reconstruction?
Immediate reconstruction:
After the General Surgeon completes the cancer part of the surgery, during the same operation, the Plastic Surgeon will rebuild the breast mound lost from removing the breast. There are a number of different techniques that are available using implants alone, or your own tissue, or a combination of both. During the consultations before the surgery, the options and risks will be discussed in detail by Dr. Giuffre.
Delayed reconstruction:
The patient has undergone a traditional mastectomy with or without radiation. A number of months or years have passed following this surgery. The decision to reconstruct the breast has been delayed.
There are a number of different techniques that are available using implants alone, or your own tissue, or a combination of both. During the consultations before the surgery, the options and risks will be discussed in detail by Dr. Giuffre
+ What are the “implant” techniques for breast reconstruction?
For either an immediate or delayed reconstruction, where no radiation was needed, the first operation involves using an implant called a tissue expander which is placed behind the muscle and skin after the breast has been removed. Two weeks following the surgery, the tissue expander is filled with fluid (saline) in small increments to increase the size of the breast mound. This is done weekly in the outpatient department at the hospital. The patient is seen weekly and the implant filled until the desired breast mound size is achieved. The breast mound is left for 3 months to allow the tissues to get used to the stretch created by the tissue expander implant.
A second operation is then done. This involves removing the previously inserted tissue expander and placing a permanent implant (usually a silicone implant) in the same space. This is similar to a breast augmentation. Please see FAQ Breast Augmentation
The breast mounds are adjusted to create symmetry: this may involve placing an implant in the opposite breast, or using a breast lift or breast reduction technique, or any combination of the above on the opposite breast to create breast symmetry. Please see FAQ Breast Lift, FAQ Breast Reduction, FAQ Breast Asymmetry
A third operation to create a nipple is the final step in the reconstruction. This is done if the patient desires an actual nipple projection. The alternative is a nipple tattoo which creates no projection, but can mimic the size, shape and color of the nipple of the opposite breast.
** Please refer to photograph’s of Patient A and Patient E above.
+ What are the “tissue” techniques (no implants) for breast reconstruction?
Rather than using an implant to create a mound projection, there are technics to create a breast mound using your own tissue. The tissue most commonly comes from the abdomen, and less frequently the buttock or the thigh.
**Please refer to the photograph of Patient D above.
+ I have had radiation. What are my reconstruction options?
Using your own tissue for the reconstruction is an option.
If an implant technique is chosen, the radiated tissue on the chest wall is removed along the mastectomy scar, and a tissue flap from the bra line attached to the “Lat “muscle (Latissimus Dorsi Musculocutaneous Flap) is used to provide healthy skin and muscle coverage over the chest wall.
**Please refer to photographs of Patients B, C, E, & F above.
An implant (tissue expander, and later followed by a silicone implant) is then placed under this tissue to reconstruct the breast mound.
+ When can I have a nipple reconstruction?
This is done as a final step in the reconstruction. Once the breast mounds are symmetrical, a nipple can be created to provide a projection surrounded by an areola to closely match the opposite breast. This is done using all of the patients own tissue. The color of the nipple and areola can be altered using medical tattooing. The tattooing can be done 3 months after the nipple areola reconstruction healing is complete.
**Please refer to the photograph of Patient E above.
If there is no desire to have a nipple projection, but the patient wants the appearance of a nipple areola on the breast mound, an areola tattoo can be done by a medical tattooist. This produces no nipple projection, but can mimic the size, shape and color of the areola of the opposite breast.
**Please refer to photographs of Patient’s A,C,D, & G above.
If there is no desire to create a nipple projection or areola, then no further reconstruction is done.
**Please refer to photographs of Patient’s B & F above.
The Followup:
+ What happens after my reconstruction?
A routine follow-up with your General Surgeon, Family Doctor, and the cancer hospital, for breast surveillance along with self-examination, is recommended.
If an implant was used in the reconstruction, an implant exchange every 10 years is recommended.
“Life is full of choices; your character reflects those choices.”











































